Introduction
Physical therapy in Mount Airy for Pediatric Issues
Welcome to Northern Rehab’s resource about Blount’s Disease in children and adolescents.
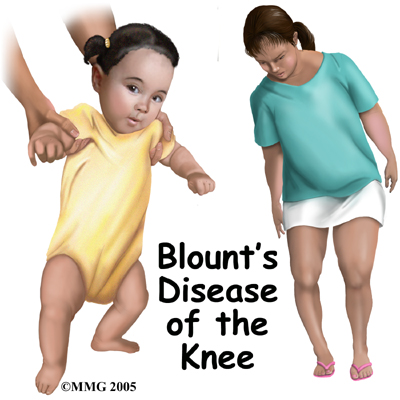
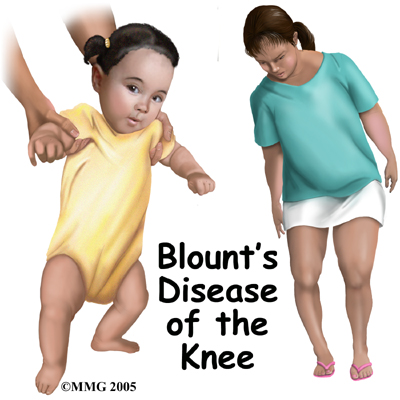
Bowlegs, also known as tibia varum (singular) or tibia vara (plural) are common in toddlers and young children. The condition is called physiologic tibia varum when it's within a normal variation and the child will grow out of it. Most toddlers have bowlegs from their positioning in utero (in the uterus). This curvature remains until the muscles of the lower back and legs are strong enough to support them in the upright position.
In some cases abnormal growth of the bone causes the bowing to get worse instead of better over time. This condition is called Blount's disease or pathologic tibia varum.
Blount's disease becomes obvious between the ages of two and four as the bowing gets worse. Overweight adolescents or teenagers can also develop Blount's disease.
This guide will help you understand:
- what part of the leg is involved
- what causes the condition
- how health care professionals identify this problem
- what treatment options are available
- what Northern Rehab’s approach to rehabilitation is
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Pediatrics|limit:15|heading:Hear from some of our *Pediatrics* patients#
Anatomy
What part of the leg is involved?
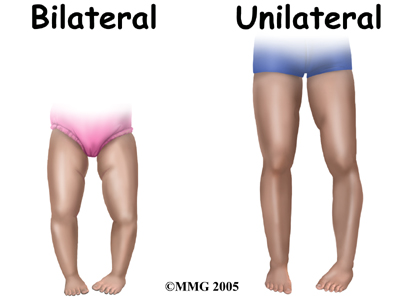
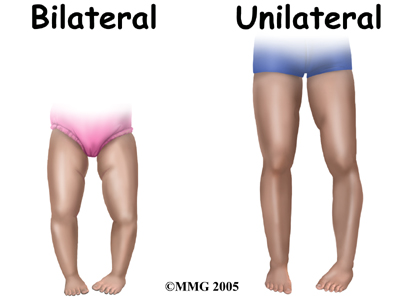
The tibia (lower leg bone) or more commonly called the shin is affected by Blount's disease. Infantile (less than three years old) Blount's is usually bilateral which means both legs are affected at the same time. The bones start to form an angle and rotate inwardly. Adolescent (11 years of age and older) Blount's is more likely to be unilateral affecting just one leg.
In the growing child, there are special structures at the end of most bones called growth plates. The growth plate is sandwiched between two special areas of the bone called the epiphysis and the metaphysis. The growth plate is made of a special type of cartilage that builds bone on top of the end of the metaphysis and lengthens the bone as we grow.
In Blount's disease the epiphysis and metaphysis both are involved. Only the medial or inside edge of the bone is affected. The metaphysis is the wider part of the tibial bone shaft. In the early stages of Blount's disease, the medial metaphysis breaks down and growth stops. In the child who is still growing, the metaphysis containing the growth zone consists of spongy bone that has not yet hardened.
Causes
What causes this condition?
There are three types of tibia varum based on the age it begins: 1) infantile (less than three years old), 2) juvenile (occurs between four and 10 years), and 3) adolescent (11 years of age and older).
Physiologic tibia varum occurs between the ages of 15 months to three years. There's no need for treatment for this normal stage of development however it is not always clear at this age if the tibia varum is physiologic (normal variation) or pathologic (Blount's disease).
Blount's disease is caused by a growth disorder of the upper part of the tibial bone.
Toddlers and children who are large or overweight for their age and who walk early are most often affected. As the child walks, the repeated stress and compression of extra weight suppresses (slows) or stops growth of the developing bone. When only one side of the tibia stops growing, there are abnormal changes in bone alignment resulting in this curvature or bowing of the bone.
There can be other causes of bowed legs in toddlers or young children. Metabolic disorders such as a deficiency of vitamin D causing rickets is more common in other countries. In the first world countries many foods are fortified with vitamin D to prevent this problem. In a small number of children, vitamin D deficiency occurs as a result of a genetic abnormality where the child cannot absorb or metabolize vitamin D.
Juvenile or adolescent Blount's disease is usually caused by obesity (being overweight) but can be the result of an infection or trauma that disrupts the medial growth plate.
Symptoms
What does this condition feel like?
 The young child may not feel any symptoms. However patients with adolescent tibia varum usually complain of pain along the medial side of the knee. The bowed appearance of the lower legs may be the first obvious sign. The child may have trouble walking without tripping. The way the child walks may not look normal. He or she thrusts the leg out away from the other leg when walking on the affected leg.
The young child may not feel any symptoms. However patients with adolescent tibia varum usually complain of pain along the medial side of the knee. The bowed appearance of the lower legs may be the first obvious sign. The child may have trouble walking without tripping. The way the child walks may not look normal. He or she thrusts the leg out away from the other leg when walking on the affected leg.
Diagnosis
How do health care professionals identify this condition?
Visual observation is the first method of diagnosis. The family or health care professional sees the problem when looking at the child or while watching him or her walk. The distance between the knees is measured with the child standing with the feet together. If the space between the knees is more than five centimeters (1 1/4 inches) further testing is needed.
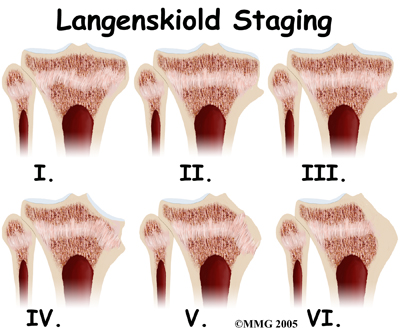
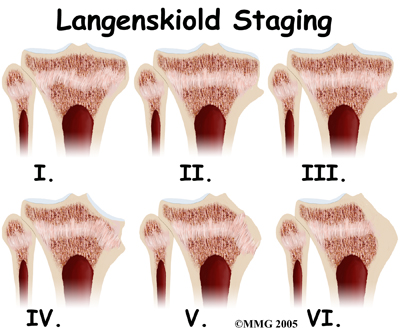
Bowing of the bones can be seen more clearly on X-rays. There are six stages of tibia varum seen on X-ray and named after the physician (Dr. Langenskiold) who first described them. The radiologist will see a sharp varus angle and other changes in the metaphysis. Often there is widening of the growth plate. The top of the tibia looks like it has grown a beak just on the medial side.
Treatment
What treatment options are available?
Treatment depends on the age of the child and the stage of the disease. Between ages birth and two, careful observation or a trial of bracing (also called orthotics) may be done. If the child doesn't receive treatment, Blount's disease will gradually get worse with more and more bowlegged deformity. Surgery may be needed to correct the problem. For the obese child, weight loss is helpful but often difficult.
Nonsurgical Treatment
Most of the time infantile bowlegs or genu varum resolves on its own with time and growth. No specific treatment is needed unless the problem persists after age two.
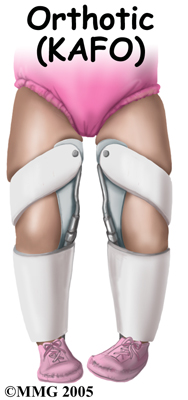
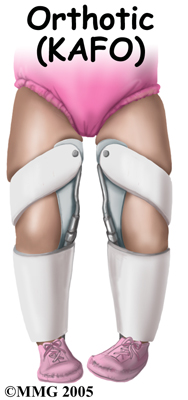
In the case of Blount's disease aggressive treatment is needed. Severe bowing before the age of three is braced with a hip-knee-ankle-foot orthotic (HKAFO) or knee-ankle-foot orthotic (KAFO). Bracing is used 23 hours a day. As the bone straightens out with bracing, the orthotic is changed every two months or so to correct the bowlegged position.
Nonsurgical Rehabilitation
What should I expect from treatment?
Your physical therapist at Northern Rehab will work with you and your child to teach you how to put on and take off the orthotic. Inspection and care of the skin is very important and will be included in the instructions given. You should watch for any blisters that develop or ‘hot spots’ which are areas of redness that indicate the brace is rubbing.
If your child is using any assistive devices, such as a walker or crutches, your physical therapist will teach your child how to properly use them and ensure they are using the most appropriate walking aid for their needs.
Your physical therapist at Northern Rehab is skilled in biomechanical assessment and gait analysis so the next part of your child’s treatment will include an analysis of their alignment and walking pattern in the brace. Adjustments to the brace may be needed. Due to muscle imbalances occurring from abnormal alignment, your physical therapist may need to prescribe some strengthening and stretching exercises to address these imbalances and encourage normal gait. If your child is young, your physical therapist will show you how to incorporate activities into your child’s daily play or normal routine that help to develop their strength and addresses imbalances. For example, we may encourage you to assist your child in stepping up and down high steps in order to gain access to a toy. This improves overall lower limb strength. You may also be encouraged to do range of motion or strengthening exercises when the brace is off, despite this time being very short. Older children will be given a more formal exercise program to address any deficits that are present.
In-toeing is often associated with Blount’s disease and this alone frequently causes children to trip and fall when walking. The combination of the orthotic and exercises will work to combat this position of the foot and improve the overall alignment of the limb. Activities that target the hip and core area will also be encouraged as these areas are the main controllers of the position of the lower extremity. Poor endurance or activation of muscles in these regions can significantly contribute to the progression of the knee deformity. Balance and coordination exercises will be combined into the activities that your physical therapist prescribes. Proprioception (the ability to know where your joints are without thinking about it) combines balance and coordination and is important in gaining maximum control over one’s joints and preventing future injuries. Exercises may include such things as encouraging your child to stand on a couch cushion while they play, or step over obstacles in order to get somewhere.
Improved strength and range of motion alone will not cure Blount’s disease, but it will make physical activity easier and may help to prevent further progression of the deformity or secondary compensation problems in the ankles, hips or low back.
If Blount’s disease in your child has been attributed to excess body weight in relation to your child’s age, your physical therapist at Northern Rehab will discuss strategies for weight loss including tips to encourage your child to be more active despite the limitations that the deformity causes. Non-weight bearing exercises that do not put excess strain on the injured joints such as swimming and cycling can be useful. If necessary, we will refer you on to a nutritionist so you can discuss a modification in caloric intake in addition to an increased physical activity regime.
Failure to correct the tibia vara deformity early often results in permanent damage to the growth plate and growing bone. Later, joint degeneration may occur. It is therefore imperative that the deformity is addressed early, and that surgical intervention is considered as a treatment option in the early stages if gradual correction does not occur.
Northern Rehab provides services for physical therapy in Mount Airy.
Surgery
Surgical correction may be needed especially for the younger child with advanced stages of tibia varum or the older child who has not improved with orthotics. Surgery isn't usually done on children under the age of two because at this young age, it's still difficult to tell if the child has Blount's disease or just excessive tibial bowing. Brace treatment for adolescent Blount's is not effective so it generally requires surgery to correct the problem.
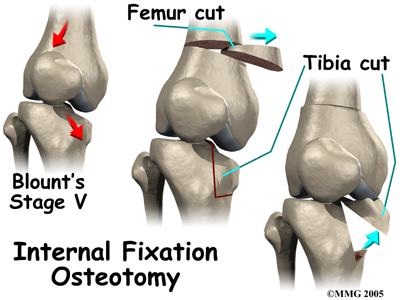
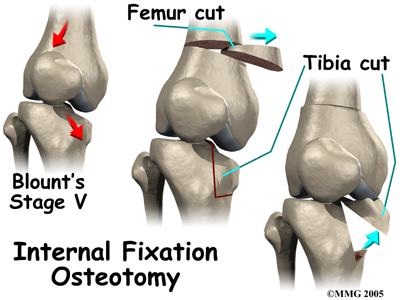
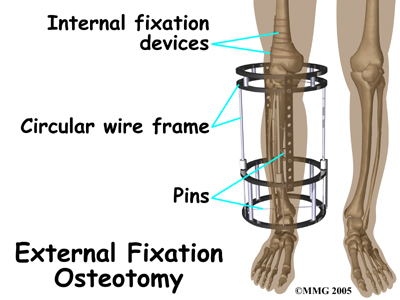
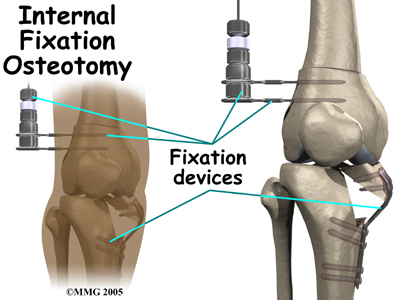
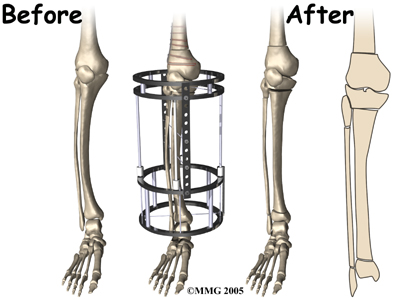
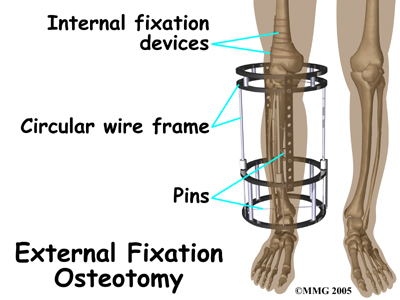
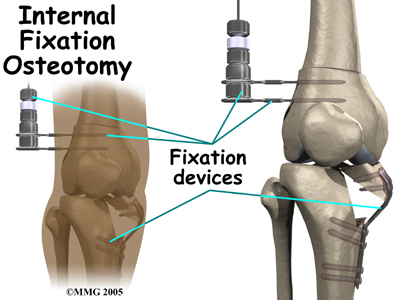
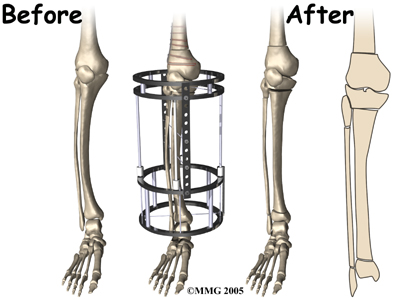
A tibial osteotomy is done before permanent damage occurs. In an osteotomy, a wedge-shaped piece of bone is removed from the medial side of the femur (thigh bone). It's then inserted into the tibia to replace the broken down inner edge of the bone. Hardware such as pins and screws may be used to hold everything in place. If the fixation is used inside the leg, it's called internal fixation osteotomy. External fixation osteotomy describes a special circular wire frame on the outside of the leg with pins to hold the device in place.
Unfortunately, in some patients with adolescent Blount's disease, the bowed leg is shorter than the normal or unaffected side. A simple surgery to correct the angle of the deformity isn't always possible. In such cases an external fixation device is used to provide traction to lengthen the leg while gradually correcting the deformity. This operation is called a distraction osteogenesis. The frame gives the patient stability and allows for weight bearing right away.
Parents or guardians should be advised that Blount's disease might not be cured with surgery. Results are usually good with infantile tibia varum. When treated at a young age and at an early stage, the problem usually doesn't come back. Older patients with advanced deformity have a much higher risk of recurrence of the deformity. Patients must be followed carefully throughout their growth and development. Unilateral bowing can result in that leg being shorter than the other leg. This is called a leg length discrepancy and may need additional treatment.
After Surgery
Osteotomy with internal fixation usually heals in six to eight weeks. The cast is removed five to six weeks after the operation if there's enough bone build-up to prevent change or loss of position. A second cast is applied that keeps the knee straight but the foot and ankle are free to put weight through the leg.
When the child has surgery with external fixators and distraction osteogenesis, gradual correction of the deformity takes place over the next three weeks. After the tibia is straightened, extra rods are used to stabilize the external frame. The frame is taken off about 12 weeks postoperatively.
Post Surgical Rehabilitation
Following surgery for Blount’s disease physical therapy treatment at Northern Rehab is very useful in returning your child to a normal activity level as quickly as possible. Physical therapy can also assist in avoiding future compensatory problems in the back or lower limbs.
Rehabilitation at Northern Rehab can begin as soon as your child’s surgeon recommends it. Each surgeon will set his or her own specific restrictions based on the child’s individual severity of deformity, the exact surgical procedure used, personal experience, and whether there is evidence that the bones are healing as expected.
The first part of our treatment will be to assist with any lingering pain there may be from the surgical procedure. Your physical therapist may use modalities such as heat, ice, ultrasound, or electrical current to aid in pain relief.
If your child is still using a walking aid such as crutches or a walking frame, your physical therapist will ensure your child is using them safely and appropriately and that they are abiding by the weight bearing restrictions set by their surgeon. We generally recommend that until it is possible to walk without a significant limp, a walking aid continue to be used. Improper gait can lead to a host of other pains in the knee, hip and back so it is prudent to continue using the aid until near normal walking can be achieved. It is expected that with young children, it is generally not possible to continue the use of the walking aid even if they would be better with it, as they will discard it as soon as they can freely move around without it.
The next part of our treatment at Northern Rehab will focus on regaining the range of motion and strength of your child’s lower limbs, and to encourage proper alignment now that the deformity has been surgically repaired. Your physical therapist may assist in stretching your child’s limbs while at the clinic and, if necessary, will ‘mobilize’ your child’s knees. This hands-on technique encourages the joints to move gradually into their normal range of motion. In addition to the hands-on treatment in the clinic we will also prescribe a series of range of motion exercises that we will encourage you to do with your child as part of their daily activity at home. Older children, as mentioned above, will be instructed to do some simple independent exercises.
Similarly to the range of motion deficits, strength deficits will also be addressed. A similar strengthening regime as that mentioned above under non-surgical rehabilitation will be used. It is pertinent to again address muscle weaknesses that have developed in the hips, core area, as well as those muscles directly around the knee. Now that a ‘new normal’ alignment has been surgically achieved, the muscles will need to be strengthened to assist in maintaining this alignment.
The final part of our Northern Rehab treatment will be ensuring that your child’s coordination and balance have returned to normal after their surgery. Following even a short period of walking with crutches and due to the surgical changes to the joint, your child’s normal balance, coordination, and proprioception can decline in function. Exercises, which may include balancing on one foot, or walking on a line or on their tippy toes, will be encouraged. More advanced exercises such as jumping, and quick agility movements will be encouraged at an appropriate time in line with the surgeon’s restrictions.
Fortunately, gaining lost range of motion, strength, and coordination after surgery for Blount’s disease goes quickly. You will notice improvements in your child’s function and gait even after just a few treatments with your physical therapist at Northern Rehab. If, however, your child’s post-surgical therapy is not progressing as your physical therapist would expect, we will ask you to follow-up with your surgeon to confirm that the knees are tolerating the rehabilitation well and ensure that there are no post-surgical complications that may be impeding your child’s recovery.
Northern Rehab provides services for physical therapy in Mount Airy.
Portions of this document copyright MMG, LLC.





 The young child may not feel any symptoms. However patients with adolescent tibia varum usually complain of pain along the medial side of the knee. The bowed appearance of the lower legs may be the first obvious sign. The child may have trouble walking without tripping. The way the child walks may not look normal. He or she thrusts the leg out away from the other leg when walking on the affected leg.
The young child may not feel any symptoms. However patients with adolescent tibia varum usually complain of pain along the medial side of the knee. The bowed appearance of the lower legs may be the first obvious sign. The child may have trouble walking without tripping. The way the child walks may not look normal. He or she thrusts the leg out away from the other leg when walking on the affected leg.